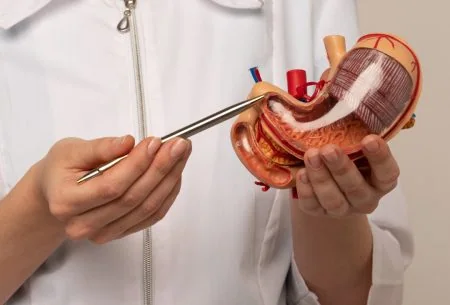
When we think of gut health, we naturally think of digestive health. But did you know that your gut also influences all your other organs, including your skin and pretty much every facet and function of your body?
Your gut microbiota (or GM for ease) is the scientific name given to the trillions of microbes, including the bacteria in your gut. And it is incredibly powerful! Thanks to this community (including 40 trillion bacteria), it is capable of thousands of functions. In fact, this newly appreciated organ is pretty much essential to whatever your health goal is, be it successful weight management, improved fitness levels, healthier skin, more resilient immunity, or even your happiness. It also has the power to influence how long you live and to protect you from over 70 chronic conditions and certain cancers.
The empowering thing is that, unlike your genetic make-up, you have the ability to shape your GM simply by how you treat it, which means that a big part of your personal health is in your hands.
Still need convincing about the importance of the gut? Let’s explore some of those gut connections that live within you.